Critical window for re-infection with HIV after stem cell transplantation
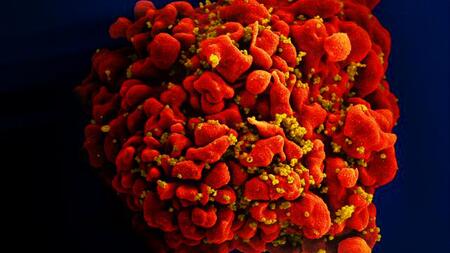
Scanning electron microscopic image of a HIV (yellow) infected T cell (red).
So far, allogeneic stem cell transplantation for the treatment of severe blood cancers has been the only medical intervention to have cured at least three people infected with the HI virus (HIV). It is still unclear why this procedure was unable to cure other HIV-infected patients successfully. In a study with 16 people infected with HIV, scientists from the University Medical Centre Hamburg-Eppendorf (UKE), the German Center for Infection Research (DZIF) and the Institut Pasteur in Paris identified a critical time window after an allogeneic stem cell transplantation, during which the expanding donor cells could be particularly vulnerable to reseeding of the HIV reservoir.
Some people with HIV need to undergo an allogeneic stem cell transplantation in order to treat different types of blood cancer. Most of the patient's immune cells are eliminated during these transplantations. Stem cells from a healthy donor are then used to replace the patient’s damaged bone marrow and restore their immune system.
“In the first weeks after an allogeneic stem cell transplantation, during which the donor’s cells and the patient’s cells still exist together, the CD4+ T cells (‘helper cells’) were strongly activated. This activation could promote reactivation of the HI virus and re-seeding of the infection in expanding CD4+ donor T-cells,” according to the study's first author, Dr. Johanna Eberhard from the UKE.
In cooperation with researchers from the Pasteur Institute, Dr. Eberhard found that new, specific T-cell responses to HIV proteins from donor cells developed after this time. This indicates that the donor cells were in contact with HI viruses during their expansion and had learnt to react against them. This confirms the existence of a “window of vulnerability” during which infection of donor cells can occur, said Dr. Eberhard.
“Together with the results of previous studies, these results show a weak point that may explain why allogeneic stem cell transplants may not completely remove the virus from the body, despite a drastic reduction in the number of infected cells. Additional immunotherapy or gene therapy may be required to achieve ongoing, spontaneous control of HIV infection in people with HIV after allogeneic stem cell transplantation,” said the co-author of the study, Associate Professor Dr. Julian Schulze zur Wiesch, senior physician in the medical clinic and polyclinic of the UKE, who carries out research with his working group at the German Center for Infection Research on topics related to curing HIV.
IciStem Consortium
The study is one of the projects being carried out by the international IciStem consortium, which has been researching the mechanisms leading to a successful decrease in the reservoir of HIV after allogeneic stem cell transplantation since 2014. The IciStem consortium (www.icistem.org) has been conducting an observational study since 2014, which includes patients infected with HIV who need an allogeneic stem cell transplant due to a serious haematological disease. The IciStem consortium consists of a European panel of experts that includes haematologists, infectiologists, virologists and immunologists.