Tuberculosis: Molecular prediction of antimicrobial resistance for tailored therapy
How can the results of molecular resistance tests be used to optimize drug therapy for tuberculosis? An international panel of experts has updated a consensus document outlining how to interpret changes in the genome of tuberculosis bacteria to derive tailored therapies for patients with multidrug-resistant tuberculosis. DZIF scientists at the Research Center Borstel, Leibniz Lung Center, have played a major role in this research.
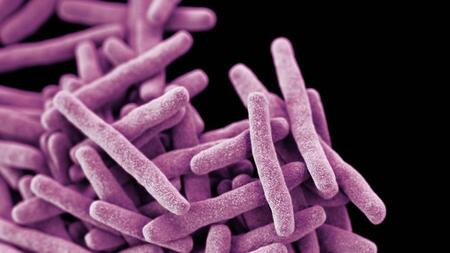
Worldwide, about 1.6 million people die from "consumption." More than from any other bacterial infectious disease. Drug-resistant tuberculosis is a growing problem for tuberculosis control. Although more effective therapies would be available for almost all patients, antibiotic-resistant pathogens are not recognized in most cases. Molecular resistance testing opens the way to rapid diagnostics and adequate therapies. The consensus has now been published in the current issue of the prestigious journal The Lancet Infectious Diseases.
The classic route of resistance testing costs too much time
To prevent the spread of tuberculosis while minimizing the emergence of bacterial resistance to available agents, affected individuals must receive rapid and adequate treatment. The classic route to adequate treatment involves the identification of tuberculosis bacteria on solid or liquid culture media. These procedures take up to eight weeks. Only then are the bacteria allowed to grow in the presence of individual antibiotics to find out which substance inhibits growth and which may not. This lengthy process means that treating physicians are "flying blind" during the first few weeks of treatment - a critical period for bringing the disease under control and preventing further transmission of the tuberculosis bacteria to others.
Molecular diagnostics shows antimicrobial resistance in a matter of days
One of the most important recent achievements in tuberculosis diagnostics has been the identification of mutations in the genetic material of the bacteria that cause drugs to become ineffective. Professor Stefan Niemann, DZIF scientist and Program Area Director at the Research Center Borstel, Leibniz Lung Center and his team have played a major role in the discovery of these mutations. Together with a group of international scientists, they have advised the World Health Organization (WHO) on the compilation of a catalog listing mutations in the DNA of tuberculosis bacteria that lead to antibiotic resistance.
Using a method that is now inexpensive, the genome of the tuberculosis bacteria of individual patients can be decoded in a matter of days. However, the information available on mutations that predict antibiotic resistance still leaves much room for discretion in selecting the right drugs for therapy in some cases.
New recommendations for therapy
An international expert panel led by Professor Christoph Lange, Medical Director at the Research Center Borstel, Leibniz Lung Center and Head of the Clinical Tuberculosis Unit at the German Center for Infection Research (DZIF ClinTB), first discussed open questions in the use of the new method in 2016 and wrote recommendations for clinical application. Since then, knowledge about the methods has expanded to such an extent that a new edition of the recommendations became necessary. Based on an extensive literature search, the panel again reached consensus on important questions about the choice of antibiotic therapy for tuberculosis, based on results of molecular predictions. The consensus has now been published in the current issue of the prestigious journal The Lancet Infectious Diseases.
"Looking into the crystal ball now works so well that, based on information from the genetic makeup of the bacteria, we are correct 99% of the time in choosing drugs for the treatment of multidrug-resistant tuberculosis," Lange explains. "The new methods offer a flexible alternative that can be established in low-resource countries and should result in each affected patient receiving individualized and adequate treatment," Lange says.