HEVbnAb: Broadly neutralizing antibodies against the hepatitis E virus
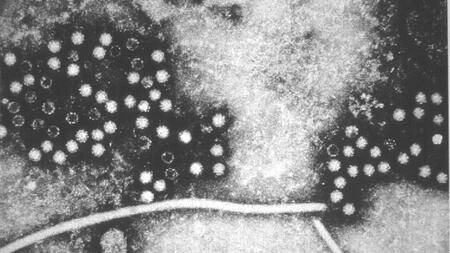
Broadly neutralizing antibodies (bnAbs) were isolated from the serum of patients who had survived acute infection with the hepatitis E virus (HEV). Several of these antibodies recognized the HEV capsid protein pORF2, the main structural protein of all human pathogenic HEV genotypes as well as a recently emerging HEV transmitted by rats.
Further development of the most promising antibody candidate could represent a specific therapeutic option for the treatment of chronic and acute HEV infections—for example, in pregnant women or patients with decompensated liver damage. At the same time, this antibody could serve as a prophylactic option to protect immunocompromised patients from HEV infections and the diseases they cause.
Background
The hepatitis E virus (HEV) is a non-enveloped RNA virus from the Hepeviridae family and is the most common cause of viral hepatitis worldwide. According to the World Health Organization (WHO), approximately 20 million people become infected with the virus each year. In 2015, 3.3 million of these infections were symptomatic, primarily in endemic regions of Southeast Asia, and 44,000 people died from the disease. There are four HEV genotypes relevant to humans: genotypes 1 and 2 are transmitted fecal-orally due to poor hygiene, while infections with genotypes 3 and 4 are usually caused by eating undercooked pork or by blood transfusions or organ transplants from HEV-positive donors.
In most cases, HEV infection resolves on its own. However, it can be fatal in up to 30 percent of infected pregnant women in their third trimester and can cause chronic infection in immunocompromised individuals, which can quickly lead to cirrhosis of the liver.
Two forms of virions are characteristic of HEV infection: a pseudo-enveloped form surrounded by a lipid membrane and a non-enveloped form. Another important feature in HEV-infected individuals is the presence of high concentrations of a secreted pORF2 capsid protein dimer in the blood. This dimer is believed to function as an antibody decoy.
Currently, there is no approved treatment for HEV. Off-label treatment of chronic HEV with ribavirin is often associated with severe side effects, which can lead to discontinuation of treatment or modification of the dosage. In addition, only about 80 percent of chronically infected patients achieve a cure. This treatment is contraindicated for pregnant women and patients with kidney damage. New therapeutic options are urgently needed for these patients, as well as for the remaining 20 percent of chronically infected patients who cannot be treated with ribavirin.
Development
Since neutralizing antibodies can provide protection, broadly neutralizing antibodies against the HEV capsid protein represent a promising new therapeutic approach. This is where a group of researchers led by Prof. Thomas Krey, Director of the Institute of Biochemistry at the Universität zu Lübeck and scientist in the DZIF research areas Hepatitis and Infections of the Immunocompromised Host, are working together with their teams. The researchers have isolated a series of human neutralizing antibodies that target the HEV pORF2 capsid protein. They are now investigating the structure and mode of action of these antibodies in the laboratory.
Partners
- Universität zu Lübeck
- TWINCORE - Centre for Experimental and Clinical Infection Research
- Hannover Medical School
- University Medical Center Hamburg-Eppendorf