New drug candidate found against persistent intestinal pathogens
Infections with the bacterium Clostridioides difficile (C. difficile for short) frequently recur due to permanent stages remaining in the intestine. A drug that also effectively combats the permanent stages does not yet exist. A recent One Health study led by the Helmholtz Centre for Infection Research (HZI), the Friedrich-Loeffler-Institute (FLI) and the German Center for Infection Research (DZIF) now shows that the natural substance chlorotonil A can do just that. Chlorotonil A is a drug candidate that could significantly reduce the risk of reinfection with C. difficile in the future, the research team hopes. The study was published in the journal Cell Host & Microbe.
"Infection with the bacterial pathogen Clostridioides difficile can lead to severe diarrhea in humans and animals. This is especially the case if the natural gut microbiome is disturbed, for example by previous treatment with a broad-spectrum antibiotic," says Prof. Till Strowig, h ead of the research group Microbial Immune Regulation at the HZI and scientist at DZIF. "Then C. difficile finds ideal conditions in the intestine and can multiply unhindered—which leads to severe diarrhea and intestinal inflammation that can also become chronic."
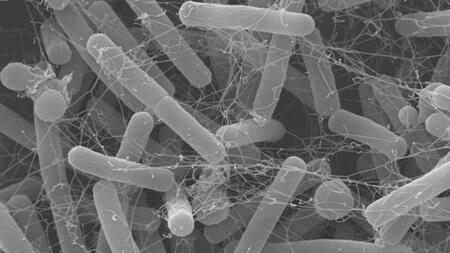
The reason for this is that the pathogen forms so-called permanent stages that remain in the intestine and can lead to a renewed infection at a later time when conditions are favourable for it. Since the C. difficile infection also requires antibiotic treatment, and the intestinal microbiome cannot recover in this way, a veritable vicious circle is created. Up to 25 percent of first-time sufferers later develop further C. difficile infections. About ten percent of the newly infected patients die as a result of the reinfection. Infection with C. difficile must be reported to the public health department in accordance with the Infection Protection Act. The pathogen is transmitted via contact infections.
"Unfortunately, the antibiotics commonly used to treat C. difficile infection today are not as effective and sustainable as one would wish. Our study addresses this problem," says Strowig, who led the large-scale multidisciplinary collaborative study together with Prof. Thilo Fuchs, deputy director of the Institute of Molecular Pathogenesis at FLI.
"We wanted to find out whether and to what extent the natural compound chlorotonil A—which is derived from a soil bacterium—is effective against C. difficile, and furthermore, how it affects the gut microbiome," says Fuchs.
At the Helmholtz Institute for Pharmaceutical Research Saarland (HIPS)—a site of the HZI in collaboration with Saarland University—intensive research has been conducted on chlorotonil A (ChA) and its chemical variants for more than ten years in order to improve them as potential pharmaceutical agents and optimise them for possible future use in humans. Against a backdrop of increasing resistance, the development of new antibiotic agents is urgently needed, and the researchers see the chlorotonil variants as promising drug candidates.
"ChA has a broad antibiotic spectrum of activity against Gram-positive bacteria and, for example, effectively combats the hospital germ Staphylococcus aureus, also known as MRSA (short for methicillin-resistant Staphylococcus aureus). In addition, ChA is also effective against the malaria pathogen," says Prof. Rolf Müller, Managing Director and head of the department for Microbial Natural Products at HIPS and coordinator of the research area New Antibiotics at DZIF. "For our study, we put the two drug candidates ChA and chlorotonil B1-Epo2 into the running. We were interested in how their efficacy compared to that of the antibiotic vancomycin, which is frequently used for C. difficile infections."
For their investigations, the research team used a wide range of methods and combined the expertise of all the research institutions involved. Microbiological methods, animal models and state-of-the-art molecular biology methods (multi-omics) were used.
"The multidisciplinary approach of our study was crucial in enabling us to achieve such comprehensive and highly satisfactory results," says Strowig. His colleague Fuchs adds, "A special feature of our study was the complementary integration of all data into a model that can facilitate the control of zoonotic diseases."
In microbiological studies, the researchers found that the two chlorotonil variants were similarly effective against C. difficile as vancomycin. ChA proved equally effective in the mouse model. "In the series of experiments with the mice, the antibiotics were discontinued after some time—and then the surprise effect occurred," says Arne Bublitz, a doctoral student in the Department of "Microbial Immunology" at the HZI and first author of the study. "The majority of mice previously treated with vancomycin became ill again. In contrast, of the mice treated with ChA, not a single mouse had reinfection."
What exactly was behind this? Bublitz pursued this question in further microbiological investigations. He treated permanent stages of C. difficile with ChA and then tried to bring them to life by creating the ideal conditions for the bacterium. But it didn't work: no viable bacterial cells developed from the treated spores. And even in mice infected with ChA-treated permanent stages, the disease was significantly attenuated.
"We were able to find out by washing with solvents that the active agent ChA most likely lodges in the water-repellent envelope of the permanent stages and forms a kind of drug depot there," Bublitz explains. "If the cell begins to germinate, it thus comes into contact with the stored ChA and dies. ChA is one of the first examples of an antibiotic that can effectively combat both bacterial cells and permanent stages in vivo at low effective concentrations."
Another research focus of the study was on the effects of ChA on the microbiome. To this end, an FLI research team conducted studies on pigs, whose digestive systems are very similar to those of humans.
"Using a wide range of multi-omics methods, we were able to show that ChA was significantly less damaging to the pig microbiome than other antibiotics," says Fuchs. "In addition, ChA had a significant negative effect on gene regulation of the intestinal pathogen."
Strowig adds: "And we also obtained encouraging results in the mouse model: After ChA administration, the gut microbiome recovered faster than it did when other antibiotics were administered. So ChA actually seems to act very specifically and to disrupt the microbiome very little in terms of its protective function." In this context, both scientists emphasise that the active agent ChA does not alter the concentration of intestinal metabolites such as proline or short-chain fatty acids, which promote the growth of C. difficile—unlike what is the case with conventional antibiotics.
Chlorotonil variants are promising drug candidates for the treatment of C. difficile infections—the results of the study clearly show this. "In particular, the effect of ChA on the permanent stages that lead to new outbreaks of disease could represent a milestone in the treatment of C. difficile infections," says Strowig. "We hope that our study will help advance natural product-based drug discovery to uncover new effective agents to fight infectious diseases. After all, they may be able to attack pathogen targets that have been inaccessible with known agents."
Source: Press release of the HZI (in German)