PANTIPA: Monoclonal antibodies targeting Pseudomonas aeruginosa
Pseudomonas aeruginosa is a multidrug-resistant bacterium that can cause life-threatening infections, such as sepsis and pneumonia. One of the key weapons used by this bacterium is the type III secretion system (T3SS), which contains the protein PcrV. Researchers at the DZIF discovered that chronically infected patients develop highly effective antibodies against PcrV. Building on this finding, the researchers produced monoclonal antibodies (mAbs) that block the T3SS and neutralize P. aeruginosa's virulence. The PANTIPA project aims to further develop the most effective patient-derived mAb candidates for clinical use against P. aeruginosa infections.
Background
Antibiotic resistance is one of the greatest challenges facing modern medicine. Pseudomonas aeruginosa, in particular, is a notorious multi-resistant pathogen that often evades conventional antibiotic therapies, causing difficult-to-treat infections. It can cause life-threatening infections, such as pneumonia, wound infections, or sepsis, in severely ill or immunocompromised patients. The World Health Organization (WHO) considers P. aeruginosa one of the pathogens for which new treatment options must be developed urgently.
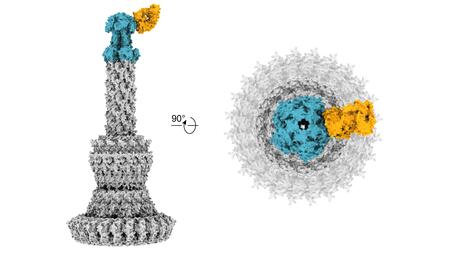
One particularly dangerous mechanism of P. aeruginosa is the type III secretion system (T3SS). This system enables the bacterium to inject toxic proteins directly into human cells, worsening the course of the disease. A central component of the T3SS is the protein PcrV, which acts as a "key" for the bacterium's attack. Blocking PcrV renders the T3SS harmless and reduces the bacterium's dangerousness.
Development
Researchers at the DZIF discovered that people infected with P. aeruginosa for an extended period produce highly effective antibodies against PcrV. These antibodies are natural defenses produced by our immune system that can recognize and neutralize specific pathogens or their components. Based on this finding, monoclonal antibodies (mAbs) that directly target PcrV were produced in the laboratory. Initial studies show that these mAbs can completely block the effect of T3SS and act similarly to antibiotics in animal models.
The project has a two-stage approach. First, an optimal mAb candidate will be selected through extensive in vitro and in vivo pharmacokinetic and efficacy studies. The first phase of the project will identify the most promising monoclonal antibody against P. aeruginosa. Several antibody candidates will then be tested in various mouse models to evaluate their efficacy against lung, bloodstream, and soft tissue infections. Meanwhile, researchers will investigate how the antibodies are distributed in the body, how long they remain effective, and whether side effects occur.
Then, the best candidate will be tested against numerous clinical Pseudomonas isolates to ensure that it remains effective against different bacterial strains. Additionally, the researchers will observe whether resistance can develop during treatment. At the same time, a comprehensive market analysis will be conducted to evaluate potential applications from an economic perspective. This analysis will be conducted in close coordination with the DZIF's Product Development Unit, which is involved in project management.
Additional funding has been secured for further project development:
- The research project is receiving €5.4 million in funding in the first round of the "GO-Bio next" program run by the German Federal Ministry of Education and Research (BMFTR).
- The ForTra gGmbH for Research Transfer of the Else Kröner-Fresenius Foundation (EKFS) is supporting the GMP-compliant production of the antibody with €1.2 million. GMP (Good Manufacturing Practice) describes strict quality standards mandatory for drug production.
- Additionally, the EKFS is providing €350,000 through its "Translational Research" funding line to prepare for a Phase I study, which will test the antibody in humans for the first time.
GMP production is currently planned to start in the first quarter of 2026.